

How Microservices Improve Healthcare Interoperability






Healthcare systems remain fragmented, with legacy monoliths, siloed departmental applications, and inconsistent data formats hindering seamless information flow.
These isolated systems restrict care coordination, complicate analytics, and slow digital innovation. Complex vendor ecosystems and limited standardization further amplify integration challenges, making interoperability a persistent barrier to efficient, patient-centric healthcare delivery.
Microservices decompose healthcare applications into modular, independently deployable services that communicate through standardized APIs. Combined with FHIR and HL7, they enable consistent data models, real-time exchange, and flexible integrations across EHRs, devices, and third-party systems.
This architecture reduces coupling, eliminates silos, and supports scalable, interoperable, and future-ready healthcare platforms.
This guide explains the advantages of microservices, when and why healthcare organizations should adopt them, key architectural and implementation practices, integration strategies, risks, and mitigation approaches.
Microservices architecture structures healthcare applications as a suite of small, autonomous services, each responsible for a single business capability, communicating through lightweight APIs or events.
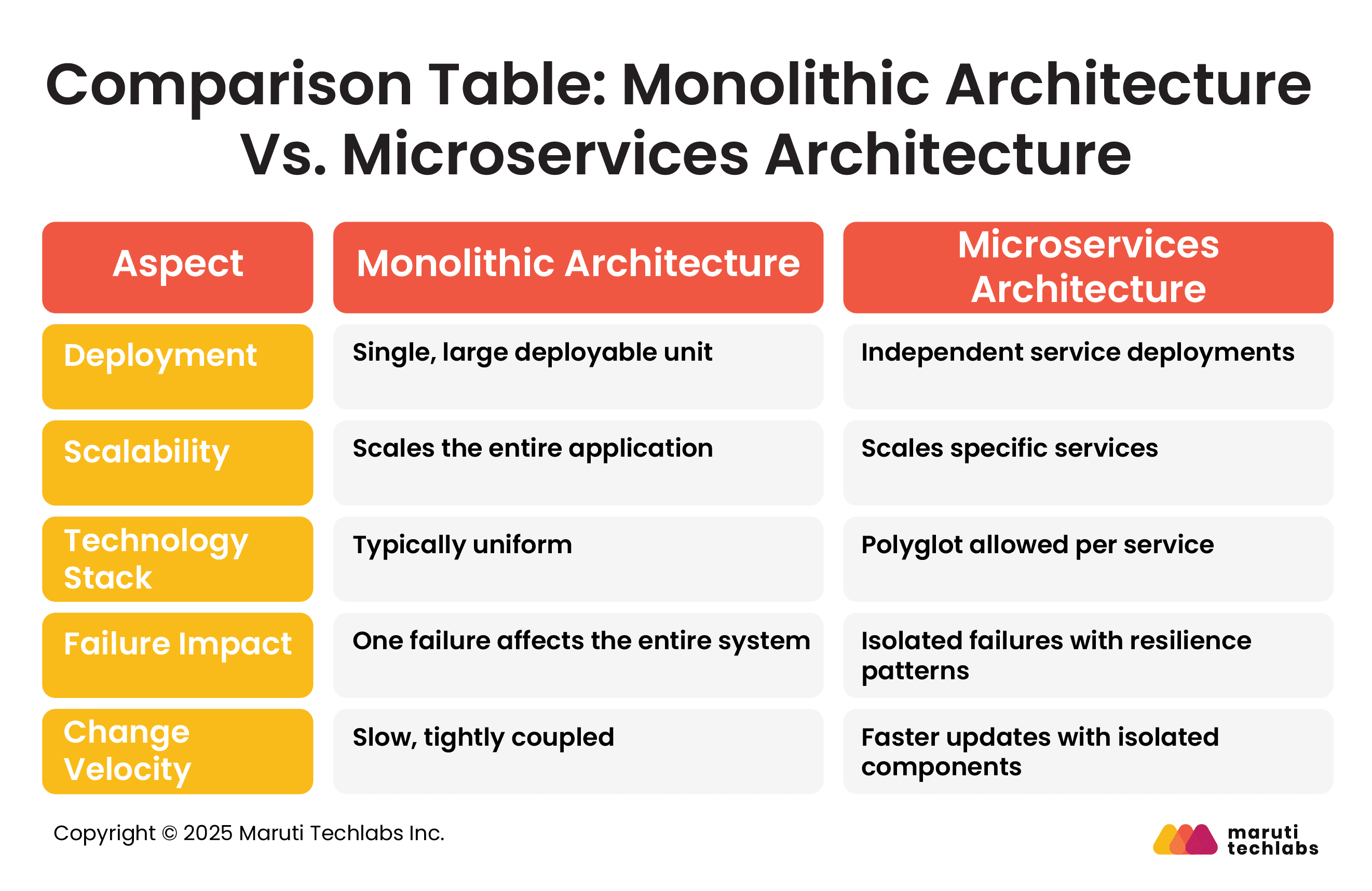
Microservices follow a modern software design approach, offering small, independent, and loosely coupled services. Each service caters to a specific business requirement and uses APIs to communicate with other services. This enables higher flexibility, scalability, and maintainability compared to monolithic architectures.
Patients' evolving expectations pave the way for rapid digital transformation in the healthcare industry. With advancements in treatments, diagnostics, and medical procedures, implementing robust technology is the need of the hour.
The inherent limitations of monolithic architectures often prevent them from adapting to these changing needs. Systems integrating seamlessly with emerging technologies like electronic healthcare systems (EHR), telemedicine, wearables, and AI-based diagnostics are direly needed. Microservices provide healthcare systems with the agility to meet growing demands.
Here is a brief list of technologies that assist with implementing microservices.
It’s a comprehensive framework that provides consistency and ease with integration when designing, developing, and documenting RESTful APIs.
A query language that offers flexibility and accurate data retrieval to address changing client requirements.
Containerization techs make deployment consistent across different environments by packaging the application and its dependencies.
An orchestration platform that simplifies microservices deployment by managing containerized applications using automated scaling, deployment, and management.
A distributed streaming platform that ensures reliable communication between microservices for real-time data pipelines and streaming applications.
A message broker that provides data exchange and seamless communication between microservices.
Healthcare systems evolve rapidly with new clinical workflows, medical devices, reimbursement models, and regulatory mandates. Modularity ensures components can be updated independently without destabilizing core systems.
API-driven design simplifies exchanging data across EHRs, devices, partner networks, and analytics platforms, enabling seamless integrations and rapid adaptation to emerging healthcare and compliance requirements.
Microservices are not universally appropriate; assessing organizational scale, integration demands, compliance requirements, and engineering maturity helps determine whether the architecture aligns with your strategic healthcare technology roadmap.

Large healthcare platforms encompassing EHRs, billing, laboratory systems, telemedicine, appointment scheduling, pharmacy, imaging, and analytics benefit from microservices.
Modularization prevents bottlenecks, supports independent evolution, and enables dedicated teams to manage distinct clinical or administrative capabilities without disrupting the broader ecosystem.
Healthcare organizations frequently integrate legacy systems, partner networks, laboratories, payers, health information exchanges, and medical devices.
Microservices, combined with standardized APIs and data models, simplify these connections, reduce point-to-point integrations, and support scalable, reusable interfaces for cross-organizational data exchange and digital health collaboration.
Microservices are well-suited to workloads with unpredictable peaks, such as appointment-scheduling surges, telehealth traffic, imaging data pushes, or multi-facility environments.
Independent scaling and elastic infrastructure ensure consistent performance, even during sudden demand spikes, without requiring complete system overprovisioning.
Healthcare organizations facing frequent regulatory changes, clinical workflow updates, or feature additions, including AI engines, decision-support tools, or remote monitoring capabilities, benefit from microservices.
Independent services allow faster releases, safer experimentation, and modular deployments without destabilizing mission-critical systems.
Successful microservices adoption requires DevOps maturity, automated infrastructure, robust monitoring, and experience managing distributed systems.
Teams must handle service discovery, observability, CI/CD pipelines, and incident response. Without these capabilities, microservices may increase operational burden instead of enabling flexibility and velocity.
Effective healthcare microservices architecture demands thoughtful data governance, integration patterns, API standardization, and versioning strategies to ensure continuity, performance, and interoperability across complex clinical ecosystems.
Shared databases simplify data consistency but reduce autonomy and complicate scaling. Database-per-service enhances independence but requires strong governance for consistency and compliance.
Hybrid models balance autonomy with shared clinical repositories. Healthcare must consider data sovereignty, auditability, performance, and regulatory constraints when selecting an approach.
Orchestration centralizes workflows but can introduce coupling. Event-driven architectures enable loosely coupled, reactive systems ideal for clinical updates and device data streams.
Hybrid models use orchestration for deterministic flows and events for asynchronous updates, delivering flexibility while maintaining reliability and traceability.
An API gateway centralizes authentication, routing, throttling, and monitoring. Rigorous versioning ensures services evolve without disrupting consumers, while backward compatibility safeguards integrations with EHR modules, partner systems, and device interfaces. These practices maintain stability during continuous service evolution.
Standardizing data exchange using FHIR, HL7, and canonical models reduces mapping efforts, enhances semantic consistency, and accelerates onboarding of new partners or devices. Canonical models act as an intermediary representation that harmonizes data across diverse systems, supporting analytics, interoperability, and regulatory reporting.
Implementing microservices in healthcare requires a deliberate combination of standardized data models, scalable integration patterns, automated infrastructure, and embedded security controls to ensure reliable, compliant, and interoperable service-to-service interactions.
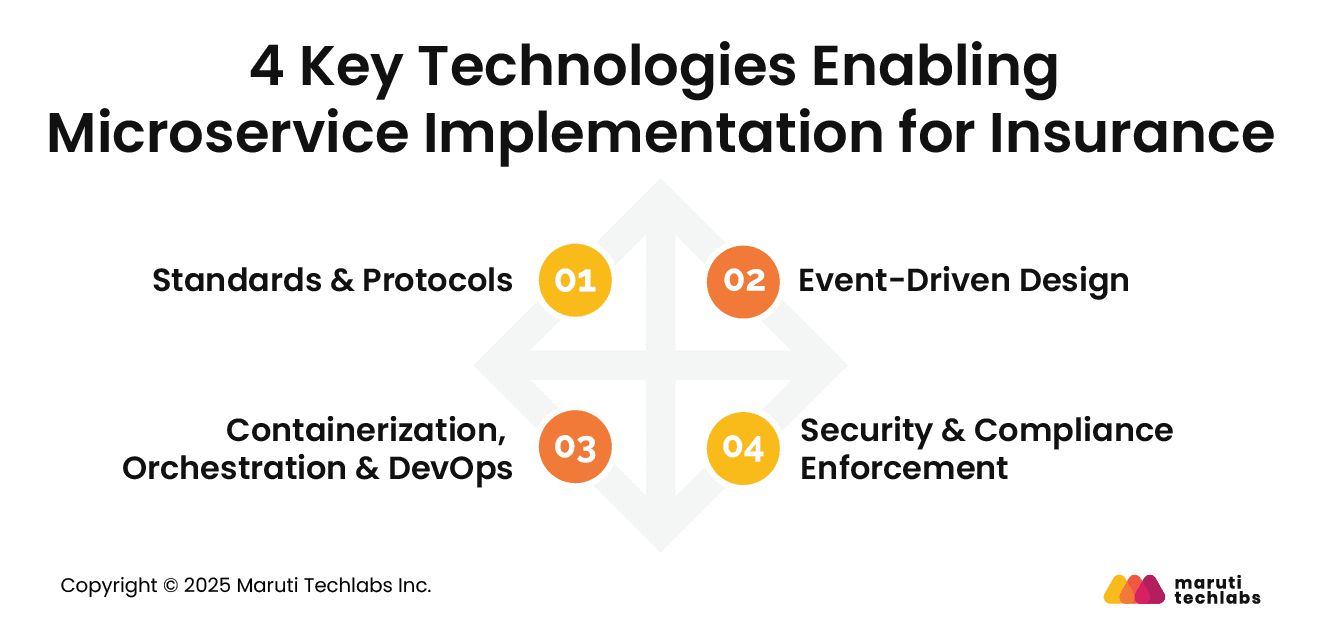
FHIR and HL7 provide structured, interoperable formats for exchanging clinical and administrative data. Terminologies like ICD-10, LOINC, and SNOMED establish universal clinical vocabularies.
Together, they enable consistent interpretation of patient information across disparate systems, supporting accurate documentation, analytics, billing, interoperability, and coordinated care delivery across organizations and digital health ecosystems.
An API-first approach ensures each service exposes clear, documented RESTful endpoints for synchronous interactions. Event-driven designs use message queues or event buses for asynchronous communication and real-time updates.
These patterns reduce coupling, enable reactive behaviors, improve scalability, and support reliable data synchronization across EHR modules, devices, and external healthcare systems.
Containers package services with all dependencies for repeatable deployments. Kubernetes orchestrates container lifecycles, scaling, and failover.
CI/CD automates testing and releases, while logging and monitoring ensure visibility into service performance. Together, these practices deliver resilience, rapid iteration, and operational consistency across large healthcare microservices ecosystems.
Healthcare microservices require strict access controls, encryption in transit and at rest, continuous audit logging, and automated compliance checks aligned with HIPAA, GDPR, and regional standards.
Per-service security isolates risks, ensures patient data protection, and supports secure integrations with external providers, payers, devices, and third-party digital health platforms.
The healthcare industry relies on seamless data exchange between systems, including EHRs, billing platforms, and clinical applications. Traditional monolithic architectures struggle with scalability, integration, and compliance.
Microservices offer a modular approach, breaking down large systems into smaller, independent services. This enhances interoperability, security, and efficiency in healthcare IT infrastructure.
Below are the 5 key benefits of microservices for healthcare systems.
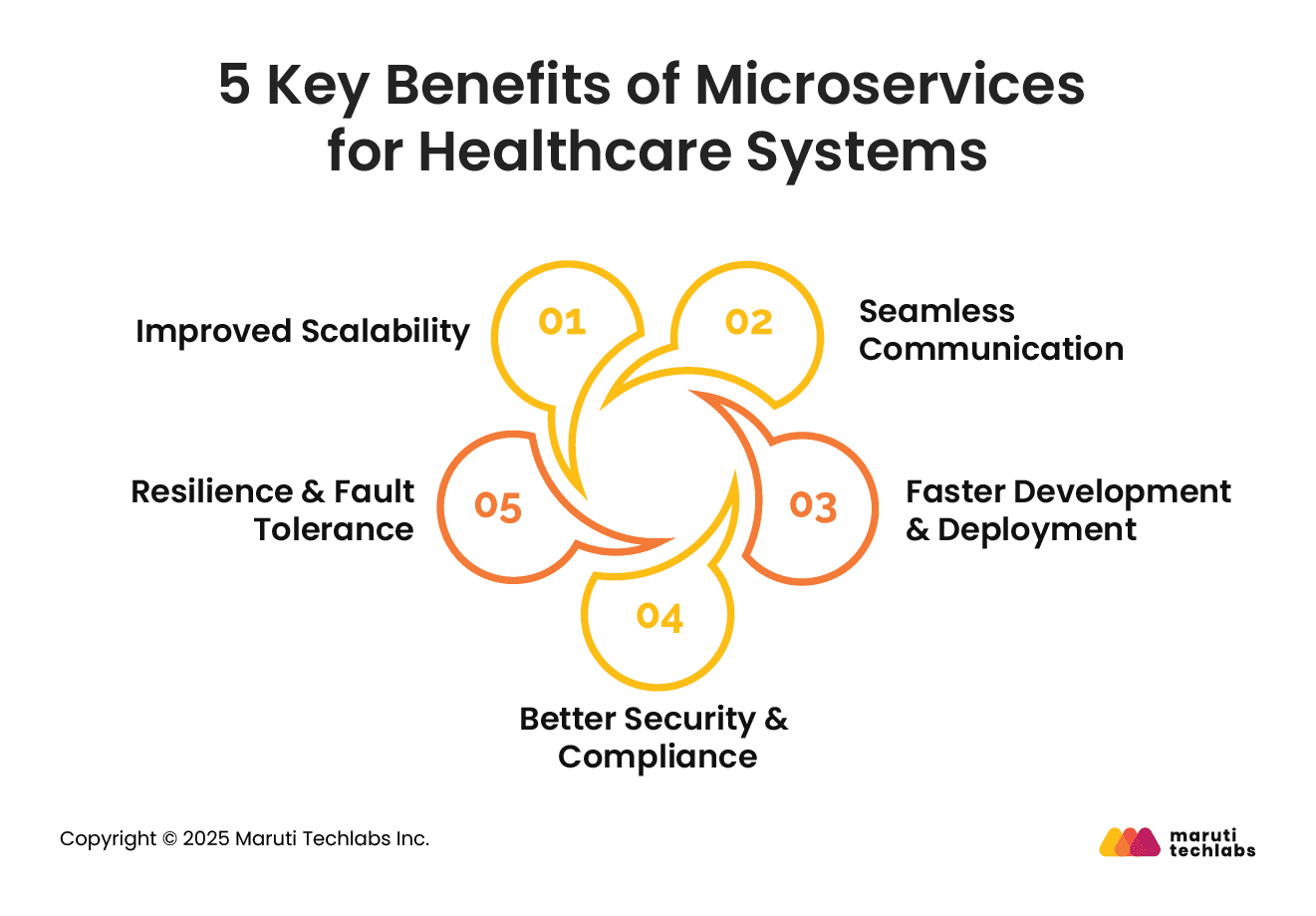
Microservices help healthcare systems scale efficiently. It allows components, such as patient records, billing, or diagnostics, to operate independently.
Unlike monolithic architectures, where scaling requires upgrading the entire system, microservices facilitate on-demand scaling. For example, a telemedicine module can be expanded during peak hours without affecting other services.
Microservices support healthcare interoperability with seamless communication between different applications via APIs.
Standards like FHIR and HL7 exchange patient data securely across platforms. This ensures that hospitals, clinics, and pharmacies can share and access real-time patient information, reducing duplication and improving care coordination.
With microservices, healthcare applications can be updated, deployed, and maintained independently. This modular approach allows development teams to implement changes in one service without disrupting the entire system.
This agility reduces downtime and accelerates the rollout of new features, such as AI-driven diagnostics or mobile health applications.
It enhances security by implementing role-based access and encrypted communication for each service.
Compliance with regulations such as HIPAA and GDPR becomes more manageable as security policies can be applied at a granular level. Data breaches are minimized since sensitive information is compartmentalized rather than stored in a single, vulnerable system.
Unlike monolithic systems, microservices isolate failures to specific components. For instance, if the billing service crashes, the patient record system remains operational.
This ensures higher system availability and minimizes disruptions in critical healthcare workflows.
Despite its advantages, microservices introduce architectural complexity, operational overhead, and new risks that must be systematically addressed through governance, automation, and robust engineering practices.
Distributed architectures increase complexity in service discovery, configuration, monitoring, and cross-service testing.
Latency, dependency chains, and version drift require sophisticated observability, automated testing, and resilient design patterns such as circuit breakers and retries to maintain reliability.
Microservices complicate the consistency of clinical data across transactions and boundaries.
Strategies such as event sourcing, sagas, compensation workflows, and canonical data models preserve integrity while enabling eventual consistency. Strong validation and audit controls ensure clinical accuracy and traceability.
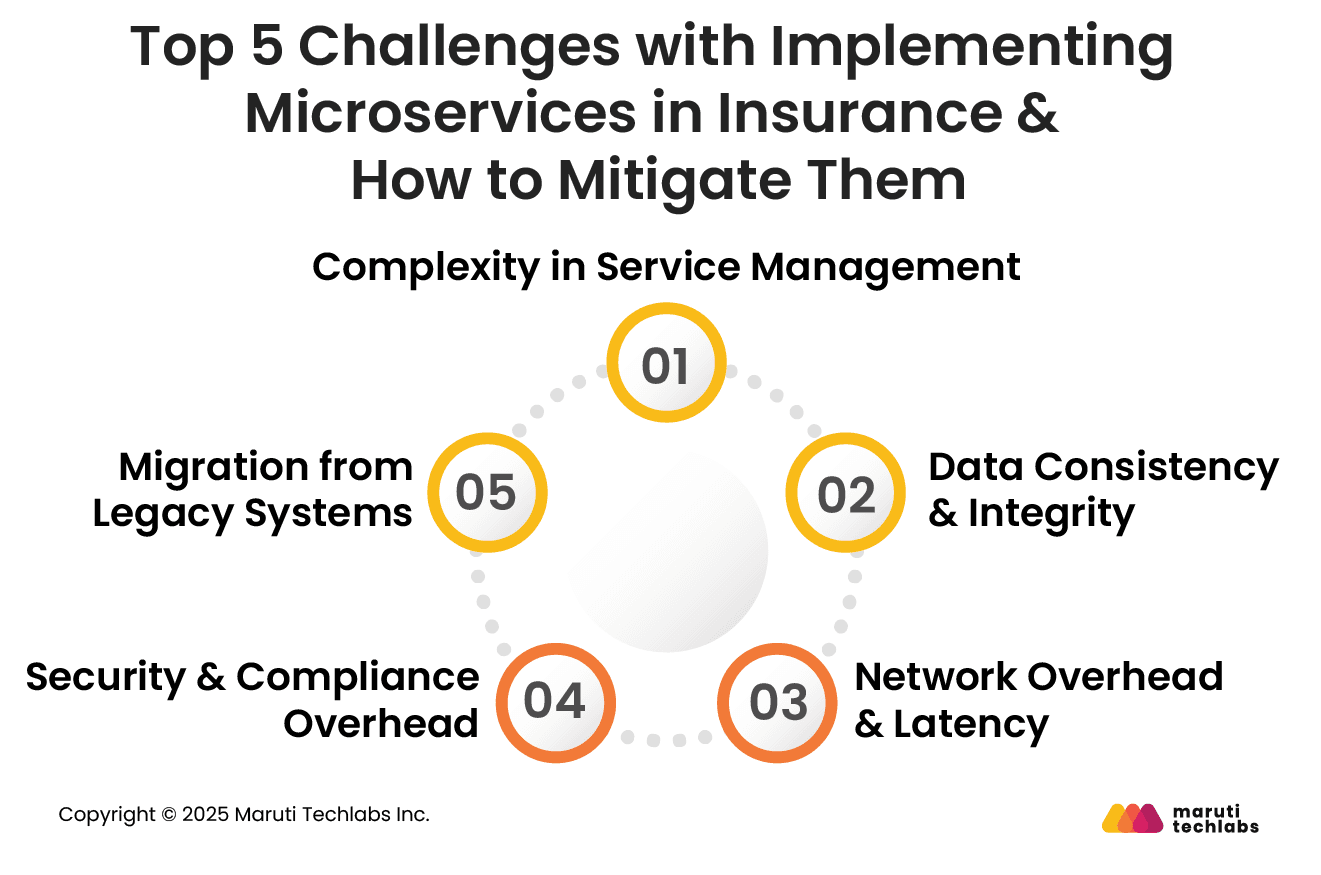
Inter-service communication increases network traffic and latency. Optimizing API design by using asynchronous messaging, caching, and co-locating related services mitigates performance issues.
Load balancing and service mesh technologies further enhance reliability and reduce communication bottlenecks.
More services expand the attack surface. Enforcing encryption, identity and access management, audit trails, and automated compliance controls is critical.
Zero-trust principles, continuous monitoring, and centralized policy management ensure secure operations across multi-institution and third-party integrations.
Transitioning from monoliths involves data migration, refactoring, parallel operations, and phased rollouts. Backward compatibility layers, strangler-fig patterns, and robust testing minimize disruption. Clear migration roadmaps and strong governance ensure safe, incremental modernization without compromising operational continuity.
Here are the top 4 most prevalent challenges observed when switching from monolith to microservice architecture.
In monolith systems, all components share a single database. On the contrary, microservices have individual databases to ensure decoupling. This demands reshaping the entire application’s data architecture.
Execute a thoroughly planned data migration strategy. You can start by breaking monolithic databases into smaller, service-specific databases.
Implement data synchronization and database refactoring techniques where required. Manage cross-service interactions using API endpoints. Additionally, data across services can be managed using methods like eventual consistency.
Usually, method calls within the same codebase facilitate inter-component communication in monolith systems. As these services are separate entities running in different environments with microservices, it is crucial to determine how they will interact.
Conduct service-to-service communication using well-defined APIs. Manage complex interactions using choreography patterns or service orchestration.
Asynchronous communication can be performed using messaging queues or protocols like HTTP/REST. Leveraging service discovery mechanisms facilitates the dynamic location of services within the systems.
Microservice-based applications are complex to deploy. Each microservice may have its deployment pipeline. Therefore, the system's distributed nature can pose a real challenge when monitoring multiple services.
Standardize deployment and scaling with orchestration tools like Kubernetes and use containerization technologies like Docker. Utilize centralized logging and monitoring tools to monitor overall system health.
Reduce human errors and enhance efficiency by maximizing automation with deployment and monitoring.
Transitioning to microservices can be challenging for legacy systems that are scarcely documented and difficult to grasp. If not managed well, this switch can pose significant risks.
Learn the intricacies of legacy systems by understanding their codebase and reviewing documents. Then, plan a stepwise transition to microservices using strategies like the strangler pattern and incremental refactoring.
Without documentation, understanding legacy systems and preventing unexpected behavior are cumbersome tasks. Mitigate these issues by implementing reverse engineering or an Anti-Corruption layer.
Here are some of the key examples of data interoperability in healthcare.
DHR is used to share patient information with other care providers. Moving patient data across healthcare ecosystems helps create a connected care environment.
HDE allows the transfer of patient data across various systems. It eliminates redundant testing and reduces administrative burden while ensuring continuity in care. Overall, DHRs contribute to creating efficient and cohesive healthcare systems.
FHIR is a standard that facilitates communication between disparate systems and electronic data sharing. It also helps integrate health information from sources like wearables and mobile apps.
It eases interpreting and using data for healthcare systems using web-based standards. In addition, it fosters accurate and timely decision-making, increasing the accessibility of patient health information. It empowers patients by giving them the convenience of portable data.
Connected healthcare platforms are essential to streamline data sharing between patients and providers and facilitate remote monitoring. This eliminates in-person visits for doctors and allows virtual consultations to manage chronic conditions.
Telemedicine platforms improve patient engagement and care coordination, offering real-time data by integrating with electronic healthcare systems. It’s also possible to link heart rate and glucose monitors and send data directly to healthcare providers, offering continuous care management.
Advanced CDSS offers healthcare professionals instant access to medication alerts, patient-specific recommendations, and evidence-based guidelines.
By integrating with EHRs, they offer safer and more personalized treatment plans. CDSS improves clinicians' decision-making by sharing crucial insights at the point of care. In addition, it optimizes clinical workflows and streamlines patient delivery.
One of our clients, Medigap Life, a Florida-based online insurance aggregator, faced challenges managing vast customer data due to rigid, interdependent workflows in its vTiger CRM. This led to performance issues and inefficiencies.
Our experts at Maruti Techlabs addressed this by migrating critical workflows to Apache Airflow, enhancing flexibility and scalability. They integrated real-time notifications from vTiger and implemented Twilio for efficient SMS communications.
This solution resulted in an 88% reduction in SMS campaign execution time and a 50% decrease in CRM page load times, enhancing decision-making with timely and accurate data.
Embracing data interoperability in healthcare is a necessity that offers significant benefits, including timely data exchange, enhanced scalability, security, and compliance.
Implementing microservices architecture is crucial for developing personalized, patient-centric, and connected healthcare ecosystems. It enables independent, modular services that enhance agility and responsiveness.
Healthcare organizations aiming to adopt microservices should begin by assessing their current infrastructure, investing in staff training, and collaborating with experienced technology partners who are experts in Microservice Architecture Development to ensure a seamless transition.
By taking these steps, organizations can position themselves to deliver more efficient, secure, and patient-focused care in an increasingly digital healthcare landscape. Get in touch with us today to start your transformation journey.
Improve healthcare interoperability by adopting microservices, standardizing data formats (FHIR, HL7), using APIs for seamless integration, ensuring security compliance, and fostering collaboration between providers, tech firms, and regulatory bodies.
Interoperability in healthcare enables seamless data exchange, improves patient outcomes, enhances efficiency, reduces errors, supports informed decision-making, ensures regulatory compliance, and fosters innovation in digital health solutions.
The four pillars of interoperability are foundational (basic data exchange), structural (standardized data formats), semantic (shared meaning of data), and organizational (policies, governance, and workflows ensuring seamless integration and use).
Data interoperability is the seamless exchange, integration, and use of data across different systems, ensuring accuracy, consistency, and accessibility for improved collaboration and decision-making.
The biggest challenge in healthcare today is ensuring affordable, accessible, and high-quality care while addressing interoperability, data security, workforce shortages, rising costs, and integrating advanced digital health technologies.


