

How to Enhance Interoperability in Healthcare Systems in 2026?






Healthcare interoperability sounds simple: share the right patient data, securely, exactly when it’s needed. In reality, that rarely happens. Information is scattered across systems, teams work with partial context, and critical details often arrive too late or not at all.
When data does not move, care slows down. Clinicians repeat tests, decisions take longer, and patients feel the impact through delays, errors, and rising costs. But when systems truly connect, everything changes. Care teams collaborate better, insights surface faster, and patients experience smoother, more coordinated care.
So why has interoperability remained such a struggle heading into 2026? Even with widespread EHR adoption, healthcare data remains fragmented. Standards such as FHIR and HL7 exist, but inconsistent implementations, vendor-specific designs, and legacy infrastructure continue to hinder seamless data exchange and meaningful reuse.
This blog explores why interoperability continues to lag, where data breaks down across the care journey, and the practical steps healthcare leaders can take to enable reliable, scalable data exchange.
Despite years of digital investment, interoperability still falls short. Let’s observe the top 5 factors that make interoperability in healthcare a huge challenge.
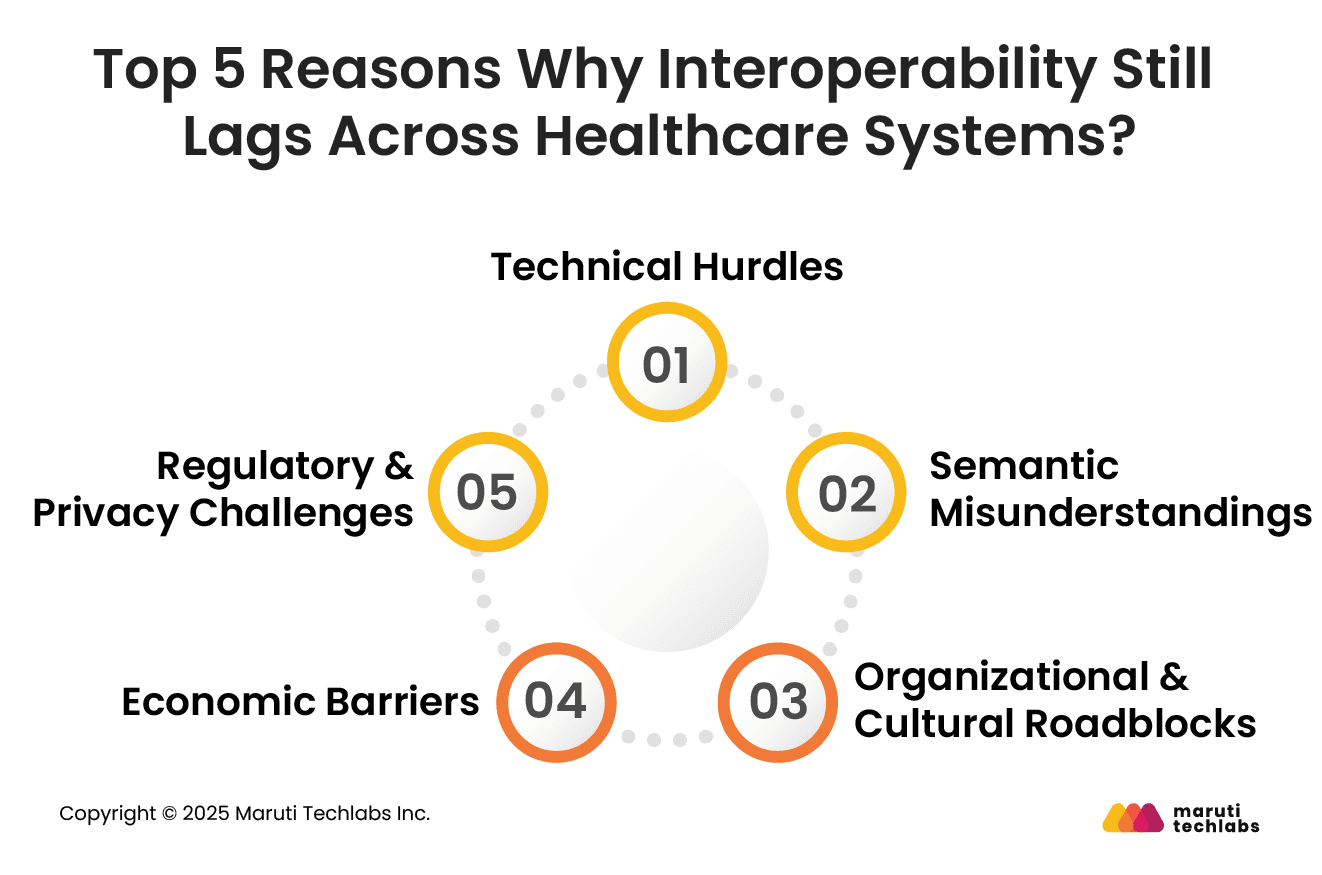
Healthcare systems frequently rely on disparate technologies built independently, resulting in incompatible data formats, proprietary systems, and legacy software that cannot easily communicate with modern platforms.
Even widely accepted standards such as HL7 and FHIR are implemented inconsistently across vendors. This demands costly custom integrations and ongoing maintenance to bridge technical gaps. These foundational technical barriers significantly slow efforts to achieve seamless data exchange.
Beyond simply connecting systems, actual interoperability demands that shared data retain consistent meaning across contexts. Variations in clinical coding, terminology, and internal data representations lead to semantic mismatches that can misinterpret information or render it unreliable.
Without rigorous semantic alignment and terminology mapping, exchanged data can be distorted, undermining trust and practical usability for clinical decision-making.
Even with technical solutions available, organizational structures and culture impede progress. Data silos persist due to resistance to change, established workflows, and reluctance to share information across departments or entities.
Information blocking, limited coordination, and inadequate training further reinforce fragmentation, reducing stakeholders' incentives and ability to adopt interoperable practices.
Healthcare interoperability efforts are costly, requiring significant upfront investment in new technology, integration tools, training, and ongoing maintenance.
Organizations face high integration costs and unclear short-term ROI, making it difficult to justify expenditures despite long-term efficiency gains. Persistent financial burdens slow adoption. In addition, it widens gaps between providers who can afford modernization and those who cannot.
Navigating the complex legal landscape of healthcare data sharing is a core interoperability challenge. Compliance with regulations like HIPAA mandates strict privacy and security protections.
They can make organizations overly cautious about data exchange. Balancing robust patient privacy safeguards with the need for seamless information flow creates friction. This is because fear of breaches and penalties leads to restrictive policies that hinder interoperability progress.
Though many healthcare providers understand the importance of interoperability, several hurdles can affect decision-making about developing an interoperable system.
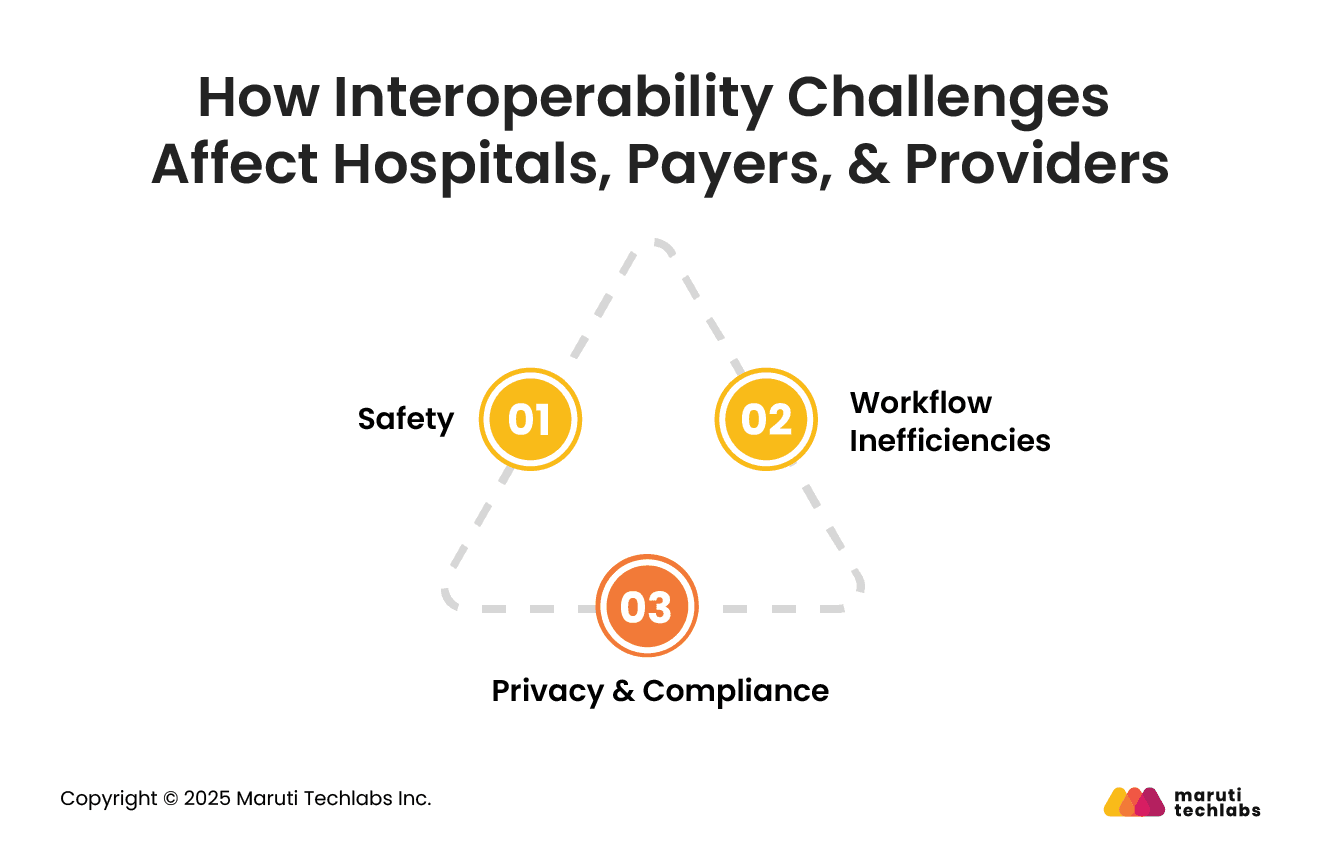
A compromised data exchange can directly affect patient safety. The risks with medical diagnosis increase when crucial medical records are fragmented or unavailable.
Inconsistent histories can result in delayed treatment, medical errors, and gaps in care coordination. Issues with interoperability in EHRs can increase costs while degrading safety.
EMRs with interoperability issues can increase medical errors by many folds. These issues can manifest into larger problems for patients and the hospitals.
Inoperable EHR systems are an evident burden for clinicians. With data fragmented across systems, physicians often face increased cognitive overload.
The excessive time clinicians spend mapping patient data across different systems contributes to burnout and diverts them from patient care. This increase in manual workload leads to wasted time and subsequently reduced job satisfaction.
Also, the unavailability of data when needed most disrupts routine patient care activities. This is the human cost of interoperability. Therefore, investing in interoperability can streamline internal workflows while enhancing your workforce’s well-being.
Managing the privacy and security of sensitive patient data is a primary challenge organizations face while implementing interoperability.
Every touch point with the system can become a source of unauthorized access. As data moves to different areas of the system, maintaining encryption, access controls, and audit trails becomes more complex. In addition, privacy concerns and data breaches pose reputational and financial risks.
Compliance adds another layer of complexity to healthcare institutions. Staying compliant with GDPR in Europe, HIPAA regulations in the US, and PHIPA in Canada, along with other regional regulations, presents different rules on where data should be stored, accessed, and shared.
Organizations can only maintain compliance with appropriate patient consent, complete documentation, and access controls. The fear of financial penalties and reputational damage can often hinder interoperability in healthcare systems.
Even with digital systems in place, healthcare data does not flow evenly from start to finish. Certain moments in the care journey are especially vulnerable to breakdowns. Here are the 5 areas where data loss occurs in the healthcare journey.
Data often fragments during registration as demographic, insurance, and consent information is captured across multiple systems.
Manual entry, duplicate records, and inconsistent identifiers create mismatches early, leading to downstream errors in eligibility checks, clinical documentation, and billing processes.
Information loss frequently occurs during transitions between providers, departments, or care settings. Discharge summaries, referrals, and test results may not transfer completely or on time.
Lack of standardized formats and real-time exchange increases the risk of gaps, delays, and clinical misinterpretation.
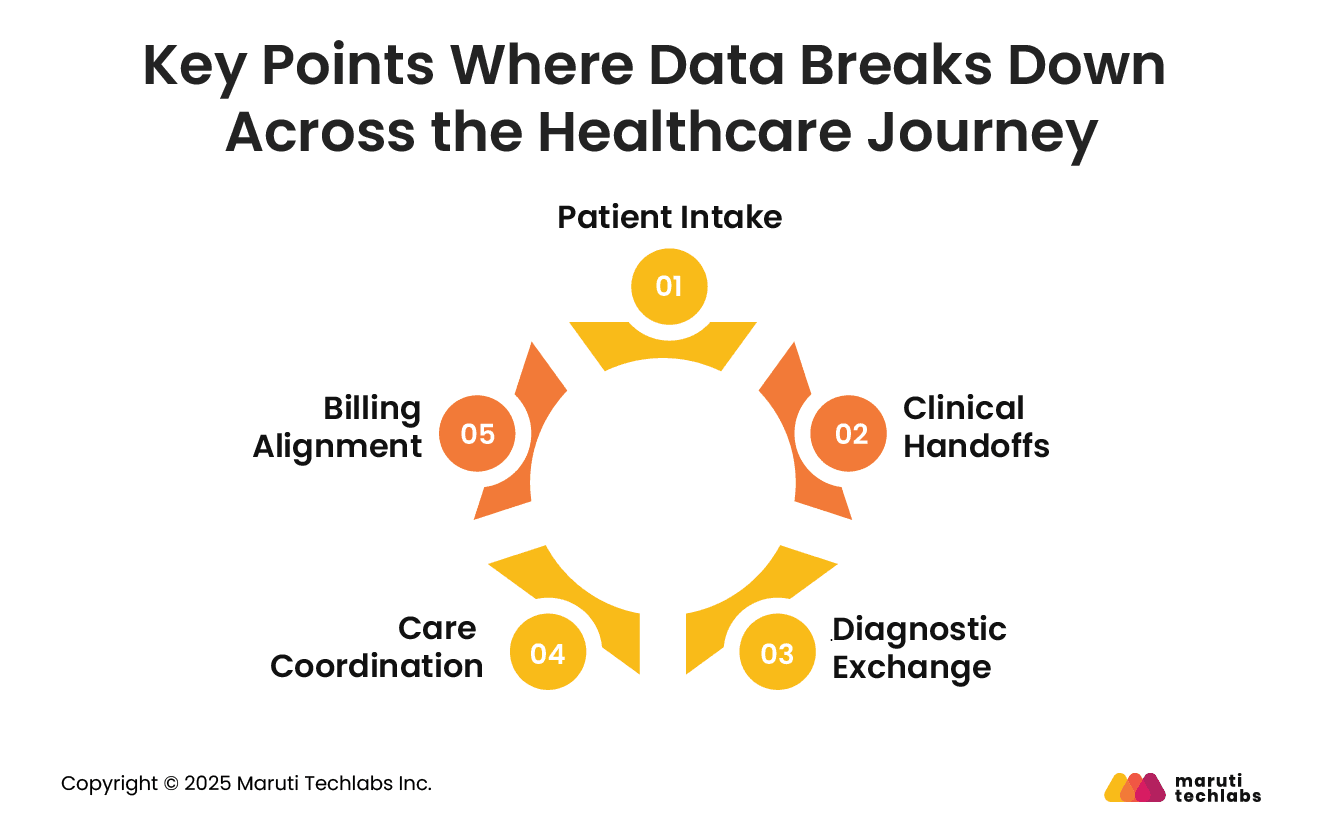
Laboratory, imaging, and diagnostic data often reside in isolated systems. Results may be shared as PDFs or faxes rather than structured data, limiting reusability.
This prevents seamless integration into EHRs, complicates longitudinal records, and slows clinical decision-making.
Chronic and complex care requires collaboration among specialists, primary care providers, and external partners. Poor interoperability restricts visibility into care plans, medications, and follow-ups.
As a result, providers operate with partial context, increasing duplication, missed interventions, and patient frustration.
Clinical and financial systems frequently fall out of sync. Incomplete or inconsistent clinical documentation leads to coding errors, claim rejections, and payment delays.
Disconnected data flows between care delivery and revenue cycle management undermine financial accuracy and operational efficiency.
Interoperability in healthcare can only be achieved if appropriate standards are met. Abiding by these standards helps exchange this data securely, clearly, and in a structured manner.
Here are the most common ones to look out for.
HL& has developed this modern standard named FHIR. It leverages technologies such as XML, JSON, and RESTful APIs to support data exchange. It’s perfect for cloud apps and mobile platforms due to its modular design, enabling the sharing of lab results or patient records.
HL7 offers widely adopted messaging standards, such as HL7 v2, and less widely adopted standards, such as HL7 v3. FHIR is a modern alternative to HL7. It primarily supports connections among different hospital system areas, such as billing, labs, and EHRs.
DICOM standardizes how medical images such as MRIs, CT scans, ultrasound, and X-rays are captured, collected, and shared. It provides consistent imaging data and metadata, enabling reliable viewing and interpretation of images across systems.
DICOM is a universal standard for handling medical imaging data. In addition to image viewing, it also ensures consistency across devices and software platforms.
Application Programming Interfaces (APIs) offer a systematic approach for systems to exchange and communicate data. This fosters real-time and secure access to patient information across the organization. Here’s how they help.
RESTful APIs are created using standard HTTP protocols around resources. This makes them a go-to choice for developers, as they are efficient for data exchange.
RESTful APIs don’t require complex parsing and return information in lightweight JSON formats that are easy to consume. These features decrease integration costs, improve development, and facilitate quick innovation.
FHIR, when equipped with the SMART framework, offers a conducive platform for launching apps within EHR systems. It drastically expands the healthcare ecosystem, allowing developers to create apps that run inside any EHR. It will enable clinicians to integrate analytics and decision-support tools directly into their workflow.
Modern interoperability is no longer driven solely by standards. It is powered by technologies that enable faster, more innovative, and more scalable data exchange.
Cloud offers the accessibility and scalability demanded by a healthcare application. Clouds fosters automatic scaling with API gateways that can process millions of applications. It supports organizations by saving vast amounts of data without significant capital investment.
By extracting structured information from unstructured notes, automating data mapping, and spotting data quality issues, AI enhances interoperability. AI-based semantic mapping can translate across various coding systems and terminology standards, reducing manual effort and improving data consistency.
As healthcare ecosystems grow more complex, interoperability remains a top strategic priority for CIOs.
In 2026, the focus shifts from theoretical standards to practical, scalable actions that enable secure, timely, and meaningful data exchange across the care continuum.
Prioritize consistent adoption of industry standards such as FHIR and HL7 across all clinical and administrative systems.
Standardized data structures and APIs reduce custom integration work, accelerate interoperability, and ensure that disparate systems can reliably share and interpret health information in real time.
Invest in clinical terminology services and master data management to harmonize vocabularies across providers.
Ensure that codes for diagnoses, medications, and procedures are mapped and validated to prevent misinterpretation. Semantic alignment is critical for accurate population health analytics and care coordination.
Enable secure, scalable APIs across core platforms to support real-time data exchange with internal and external partners.
Robust API strategies ensure flexibility for mobile applications, telehealth, and patient access while reducing reliance on batch file transfers and point-to-point integrations.
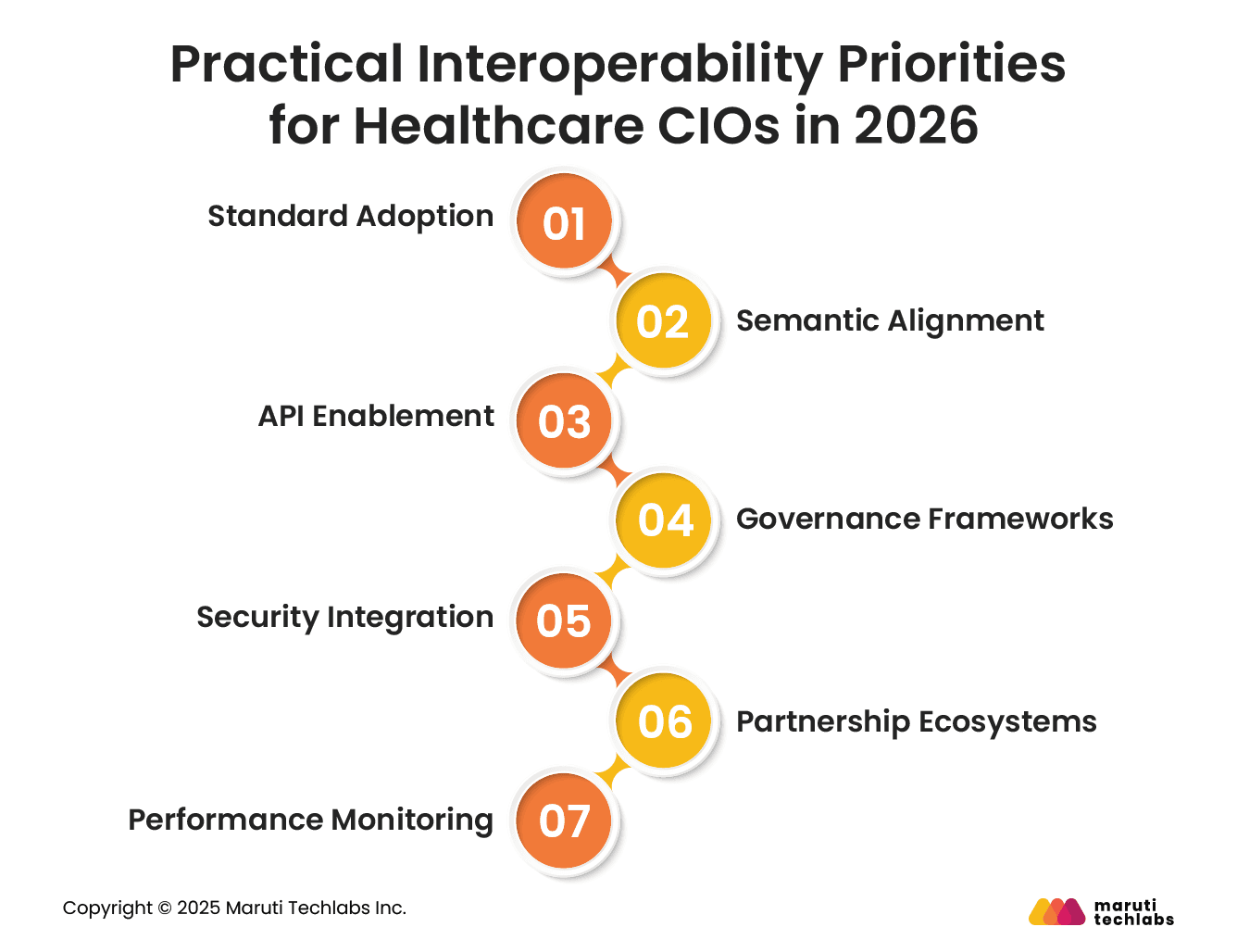
Establish strong governance to oversee data quality, access policies, and interoperability compliance.
Define stewardship roles, metrics, and escalation paths to maintain accountability. Governance frameworks ensure consistent practices and minimize risks associated with data sharing and privacy obligations.
Embed privacy and security protections into interoperability workflows. Use encryption, identity federation, and access controls to safeguard patient data.
Balance regulatory compliance with usability so that authorized partners can exchange information without risking breaches or excessive friction.
Forge strategic partnerships with health information exchanges (HIEs), technology vendors, and payers.
Collaborative ecosystems expand data reach and support unified care pathways. Shared investment in integration accelerates innovation while reducing redundancy and vendor lock-in.
Implement interoperability performance metrics and dashboards to track data exchange quality, latency, and success rates.
Continuous monitoring identifies bottlenecks, informs optimization, and demonstrates ROI to stakeholders. Data-driven insights guide resource allocation and improvement planning.
Interoperability remains healthcare’s most persistent data challenge because it is not just a technology issue. It spans legacy systems, fragmented standards adoption, governance gaps, and misaligned incentives.
As healthcare leaders look toward 2026, the focus must shift from isolated integrations to enterprise-wide data strategies built on standardized models, robust APIs, and strong data stewardship. Scalable cloud platforms and modern architectures are essential to enable real-time, secure data exchange.
An AI-ready data ecosystem depends on accessible, high-quality, and well-governed data. Interoperability is the foundation that makes this possible, enabling better care coordination, faster insights, and improved outcomes at scale.
Ready to move forward? Leverage Maruti Techlabs’ AI Strategy & Readiness services to define the right architecture, standards, and roadmap for secure, scalable transformation. Connect with us to accelerate your healthcare data and AI journey.
Improving interoperability requires a combination of standards, architecture, and governance. Healthcare organizations should adopt industry standards such as HL7, FHIR, and ICD to ensure consistent data exchange.
Modern, API-driven, and cloud-based architectures enable real-time integration across systems. Strong data governance, master data management, and security controls are essential to maintain data quality and compliance.
Finally, aligning workflows, incentives, and stakeholder collaboration ensures interoperability delivers measurable clinical and operational value.
The four types of healthcare interoperability are foundational, structural, semantic, and organizational. Foundational interoperability enables basic data exchange between systems.
Structural interoperability defines data formats and syntax, ensuring consistency. Semantic interoperability ensures shared meaning through standardized vocabularies and terminologies.
Organizational interoperability aligns policies, governance, and workflows across institutions, enabling effective data use within legal, regulatory, and operational frameworks.


